by SXHH Marketing | Feb 4, 2022 | Hormone Replacement Therapy, Menopause
If it seems like every time you look in the mirror you find more wrinkles and sagging, you might be searching for ways to stop the signs of aging on your skin. Many women experience what seems like accelerated signs of aging on their skin after menopause. However, we have some good news. Some recent evidence suggests that estrogen replacement therapy may help prevent some of the signs of aging and may promote healthy skin. Researchers are still studying the effects of estrogen on the skin, but many of the studies have been encouraging. Let’s talk about estrogen, menopause, aging, and your skin.
Why Our Providers May Recommend Estrogen Replacement Therapy

Estrogen replacement therapy may help with menopause symptoms and some studies suggest it may also help prevent some skin aging concerns.
First, let’s discuss why a hormone doctor may recommend estrogen replacement therapy. While everyone is different, one of the most common reasons our providers prescribe hormone therapy is to alleviate symptoms of menopause. Many menopause symptoms are unpleasant and can even interfere with everyday life. For instance, some of the symptoms you might experience during menopause include:
- Hot flashes
- Night sweats
- Mood changes
- Insomnia
- Low libido
- Vaginal dryness
- Weight gain
- Brain fog
Declining levels of estrogen during menopause are primarily to blame for these symptoms. Fortunately, many women find symptom relief through a hormone replacement therapy regimen. This is why our providers may recommend beginning estrogen replacement therapy during menopause.
Menopause may also have negative effects on your skin which can make you look older. For instance, after menopause skin thickness typically decreases by about 1% each year for the first five years after menopause. Collagen in your skin also tends to decrease by 2% each year for about 20 years after menopause. Low estrogen levels may also be responsible for some of these changes, which is why researchers are looking into the potential anti-aging effects of estrogen. Research is still ongoing, but much of the evidence so far is positive.
Estrogen Replacement Therapy May Have Beneficial Effects for Your Skin
There are many factors that can make our skin look older. Environmental, genetic, and hormone conditions can all contribute to common signs of aging. Declining hormone levels during and after menopause may contribute to issues like increasing number of wrinkles, deeper wrinkles, less elasticity, dryness, as well as other skin issues that tend to make us look older. There are many estrogen receptors in the skin, particularly in the skin on your face. This may explain some of the effects of menopause on your skin. However, some research indicates estrogen replacement therapy may help prevent wrinkles and other signs of aging.
For example, one 2005 study from Yale University looked at the effects of long-term estrogen therapy on wrinkles and skin rigidity. The researchers in the study found that women who used hormone therapy had fewer wrinkles, less severe wrinkles, and better skin elasticity.
This small study included eleven women who did not use hormone therapy after menopause and 9 women who did use hormone therapy long-term for menopause symptoms. All the women had similar characteristics that might contribute to wrinkles and skin rigidity, such as age, sun exposure, and tobacco use. The researchers had a plastic surgeon assess the appearance of the skin without knowing who was in the control group and who was in the hormone replacement therapy group. The women who didn’t use hormone therapy on average had more wrinkles, deeper wrinkles, and more rigid skin.
Based on the results, the researchers concluded that estrogen may promote skin health and may also prevent wrinkles and skin rigidity to help the skin look younger. While estrogen likely won’t reverse or erase signs of aging, it may offer some protection against wrinkles and other common skin concerns in menopausal women.
Estrogen’s Effects on the Skin
Estrogen may impact the look of your skin in many ways. Researchers are still studying the reasons why estrogen may prevent some signs of skin aging. Estrogen may affect skin cell production, collagen production, hydration, and thickness of your skin. All these factors can affect the appearance of your skin.
Estrogen Replacement Therapy May Improve Skin Cell Production
Some researchers believe that estrogen moderates the production of keratinocytes. These are skin cells that make up nearly 90% of the cells in the top layer of your skin. When we are young, skin cells are in a near-constant state of turnover. The dead skin cells slough off rapidly as the lower levels of your skin produce more new skin cells. However, this process tends to slow down as we age, and declining estrogen levels during menopause may play a role in this. Estrogen replacement therapy may help increase skin cell production which can reduce the appearance of wrinkles and dull skin.
Estrogen Replacement Therapy May Increase Collagen
Another way estrogen may help prevent signs of aging on your skin is through collagen production. Estrogen receptors may also act on the fibroblasts in the dermal layer of your skin. Fibroblasts are responsible for creating collagen, which provides the main support structure for your skin. As collagen production declines, the skin can start to sag and develop more wrinkles. However, estrogen may increase how much collagen your skin produces to help prevent these issues.
Estrogen May Improve Skin Hydration
Female hormones estrogen and progesterone can also improve hydration for the skin. For instance, hormones can affect how much sebum your body produces. Sebum is an oily substance that coats your skin and hair to help with moisturization and protection. As we enter menopause, sebum production can also slow down, leading to chronically dry skin. Dry skin can make wrinkles and fine lines look much deeper than they truly are. However, many researchers have found that estrogen replacement therapy can help increase hydration and moisture in the epidermis.
Estrogen Replacement Therapy May Increase Skin Thickness
Your hormones can also have a pretty big impact on how thick your skin is. Thinner skin tends to become more wrinkled, less elastic, dryer, and also more easily damaged. During our pre-menopausal years, the skin actually gets thinner at certain points of the menstrual cycle, particularly right before your period where your estrogen levels are at their lowest. Therefore, low estrogen levels during menopause may contribute to thinning skin as we age. Some studies have found that estrogen replacement therapy may increase skin thickness significantly after menopause.
Other Skin Care Tips for Menopause
Of course, there are many other things you can do to help take care of your skin during and after menopause. Estrogen isn’t the fountain of youth – even if it does help prevent some wrinkles, it isn’t a cure-all for aging. Hormones are only one part of what ages your skin over time. Embracing your skin as it changes and taking part in a good skincare regimen can also help keep your skin healthy in menopause.
For instance, you may experience dry skin after menopause. In these cases, it can help to switch to a milder cleanser and to moisturize more often and with heavier creams. Also, sun damage can lead to even thinner skin after menopause. Wearing sunscreen can help reduce sun damage that may cause issues like thinning skin, age spots, wrinkles, and even skin cancer. In addition, retinol products can help increase collagen, which may help with wrinkles or sagging skin. So, whether you’re taking bioidentical hormones for menopause or not, there are many things you can do to help your skin after menopause.
Talk to Our Health Care Specialists at HerKare
Our team at HerKare is here to help you feel like the best version of yourself. We empower you to take control of your health through convenient, affordable healthcare. We understand you want to feel and look your best at every stage of life, which is why we offer personalized care for everything from wellness exams to menopausal hormone therapy. You can trust us to listen to your concerns and work with you to find treatment options that work well for you. Make an appointment today to discuss your health and symptoms with our caring team of medical professionals.
by SXHH Marketing | Jan 20, 2022 | Menopause, Wellness
January is Thyroid Awareness Month! To help raise awareness about thyroid disease, let’s talk about thyroid disorders and menopause. Thyroid disorders are incredibly common among women, and the risk for thyroid issues increases with age. Most cases of thyroid disorders occur in middle aged women, which is also typically when menopause occurs. In some cases, you may have both at the same time. Some women mistake thyroid disorder symptoms for menopause and vice versa. Also, thyroid issues can cause worse menopause symptoms. There are many ways thyroid disease and menopause can interact, which is why it’s important to talk to our women’s health care providers about your overall health. We offer diagnosis and treatment for both thyroid disease and menopause to help alleviate your symptoms and reduce other health risks associated with both thyroid disorders and menopause.

Our women’s health care providers can help you address symptoms of thyroid disorders and menopause.
Talk to Your Women’s Health Care Provider About Your Thyroid
The thyroid is a small, butterfly-shaped gland located in the front of your neck, just above the collarbone. Its purpose is to produce thyroid hormones, which affect practically every cell in your body. Thyroid hormones are responsible for a wide range of functions in the body, including your metabolism and heart rate. The more thyroid hormone in your body, the higher your metabolism is and the higher your heart rate. However, thyroid disorders negatively affect normal functioning of the thyroid gland. Women are between five and eight times more likely than men to suffer from thyroid disorders. In fact, an estimated one in eight women will experience thyroid issues at some point in their lifetimes. Because the thyroid plays such a key role in your health, it’s important to talk to our women’s health care provider if you think you may be suffering from a thyroid disorder.
Types of Thyroid Disorders
Generally, thyroid disorders involve either an overactive or underactive thyroid. Overactive thyroids produce more thyroid than your body needs. Underactive thyroids produce less thyroid hormone than your body needs. Both can cause serious issues for your health, as well as a variety of symptoms that can interfere with your everyday life.
Hyperthyroid involves an overactive thyroid where you produce too much thyroid hormone. This essentially causes your body to speed up. For instance, with too much thyroid hormone circulating in your body, you may have an increase in metabolism to the point it creates health issues, like unexplained weight loss.
By contrast, hypothyroid is where you don’t produce enough thyroid hormone. With low thyroid, your body and its functions can start to slow down. One example is you may feel more tired than usual and feel like you need to sleep more. Just like hyperthyroidism, this can also negatively impact your health.
Autoimmune diseases are most commonly to blame for thyroid disorders in the U.S. The most common cause of hypothyroid is Hashimoto’s disease, which causes your body to develop antibodies that attack the thyroid gland. Graves’ disease is an autoimmune disease that is the culprit for most cases of hyperthyroid in America. This disease causes your body to create an antibody that actually mimics thyroid stimulating hormone (TSH), which is responsible for boosting thyroid production when your body needs more. Because the antibody acts like TSH, it causes your body to produce too much thyroid hormone.
How Women’s Health Care Providers Diagnose and Treat Thyroid Disease
If you think you may have a thyroid disorder, talk to one of our women’s health care providers. We can help diagnose and treat both hypothyroid and hyperthyroid. In most cases, diagnosis starts with a simple blood test. Blood panels may look at many factors to assess whether you have a thyroid disorder. Thyroid tests may look at the amount of thyroid stimulating hormone in your blood, T3 & T4 (types of thyroid hormone) levels, and thyroid antibody levels. Diagnosis may also include thyroid scans and ultrasounds.
If you have a thyroid disorder, our women’s health clinic can also help with treatment. Treating hypothyroid typically involves taking medications that supplement your natural thyroid hormone levels. They are generally man-made versions of thyroid hormones and come in different forms, like pills or injections. In most cases, you will need hypothyroid treatment for the rest of your life to relieve symptoms and reduce some of the risks associated with low thyroid levels.
Treating hyperthyroid means reducing how much thyroid hormone is in your body. There are many approaches to this. Treatments from your women’s health care provider may include medicines that reduce thyroid production or reduce the effects of thyroid hormone in your body. In these cases, most people need lifelong treatment. Other potential options for hyperthyroid include radiation therapy to target and kill some of the thyroid cells and shrink the thyroid gland. Another option includes surgically removing part or all of the overactive thyroid gland.
Thyroid Disease and Menopause May Share Symptoms
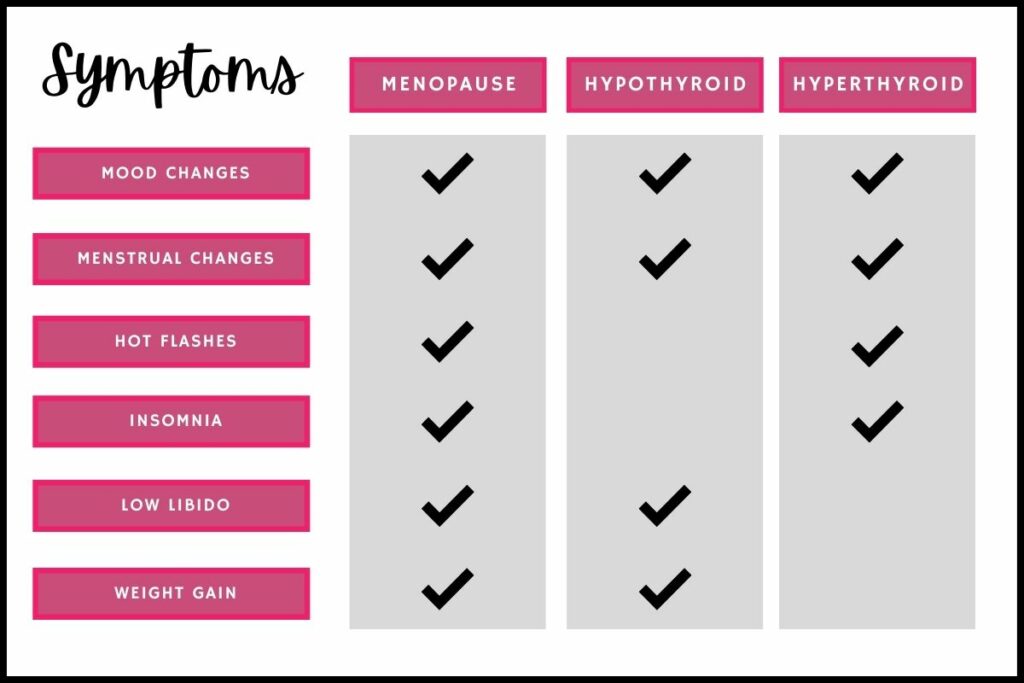
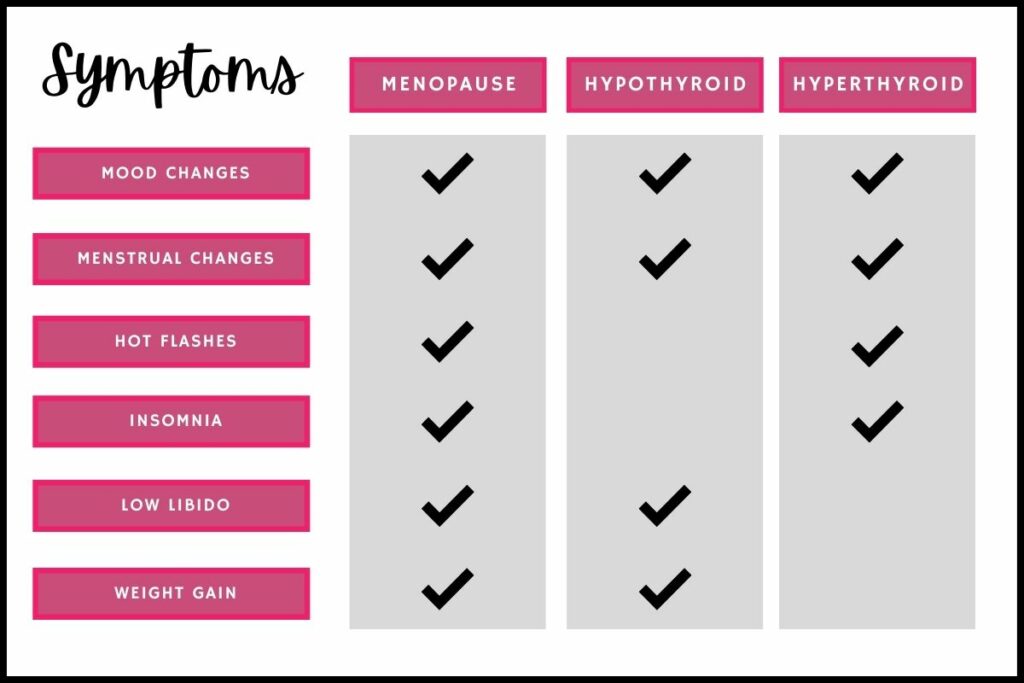 Many women mistake thyroid issues for menopause, or vice versa. Thyroid disorders can mimic many of the same symptoms of menopause.
Many women mistake thyroid issues for menopause, or vice versa. Thyroid disorders can mimic many of the same symptoms of menopause.
Some symptoms of hypothyroid include:
- Fatigue
- Cold intolerance
- Dry skin
- Constipation
- Libido changes
- Menstruation changes
- Moodiness
- Forgetfulness
- Unexplained weight gain
- Hair loss
- Depression
Some symptoms of hyperthyroid include:
- Hot flashes
- Insomnia
- Heat intolerance
- Unexplained weight loss
|
- Racing heart
Heart palpitations
Anxiety
Muscle weakness
|
You may have noticed when reading those lists that both hyperthyroid and hypothyroid have similar symptoms to menopause, namely mood changes, menstrual changes, hot flashes, insomnia, and libido changes. Many women also experience weight gain around the time of menopause, which is common for people with hypothyroid. Therefore, it may be easy to mistake symptoms of thyroid disorders for menopause.
In addition, thyroid disorders may make your menopause symptoms worse. In some cases, you may need to treat both your thyroid disease and your low hormone levels from menopause to alleviate your symptoms.
Any time you experience symptoms like temperature intolerances, hot flashes, mood changes, unexplained weight changes, or other similar symptoms, it helps to talk to your women’s health care provider. Our team can help find underlying causes of your symptoms and identify personalized treatment options that suit your lifestyle.
Talk about Risks of Thyroid Disease with Your Women’s Health Care Provider
Untreated thyroid disorders can cause major problems for your health. Thyroid disease can increase your risk for many other serious health conditions. For instance, hypothyroid can increase the risk for high cholesterol, heart disease, and depression. Hyperthyroid can also increase the risk for heart disease and may increase the risk for vision issues. One common side effect of untreated hyperthyroid is called Graves’ ophthalmopathy, which can cause eye pain, light sensitivity, double vision, and even vision loss.
Thyroid disease of any kind can increase the risk for goiter, which is where the thyroid gland becomes enlarged, even to the point where you can feel the lump in your neck or experience symptoms like difficulty swallowing, cough, difficulty breathing, and hoarseness. Our doctors are here to help you reduce your risks for your overall health and well-being.
Thyroid issues can also make menopause health risks worse. For instance, osteoporosis is a serious risk for women after menopause. Osteoporosis is where your bones become weaker and more brittle, increasing the risk for fractures. Both hyperthyroid and hypothyroid can also increase the risk for osteoporosis, making it a double whammy if you have a thyroid disorder and are menopausal. Our women’s health care providers can discuss options to help protect your bones and reduce the risks based on your specific circumstances.
Quality Health Care from HerKare – Your Women’s Health Clinic
When you need better healthcare for women, choose our team at HerKare. We are a women’s health clinic founded by and run by women, for women. We pride ourselves on offering personalized care for women. Our team offers a wide range of healthcare services, from annual exams to HRT for menopause and treatments for health conditions like thyroid disease. Our goal is to empower women to take care of themselves by making healthcare as efficient and convenient as possible. Make an appointment today to take charge of your health.

by SXHH Marketing | Dec 3, 2021 | Hormone Replacement Therapy, Menopause, Wellness
We all know exercise is important for health. Yet, many people don’t get enough exercise on a regular basis for one reason or another. Several surveys and studies have also found that women are typically much less active after menopause than before menopause. Many scientists believe this may be due to hormone changes during menopause, particularly lower estrogen levels. Researchers are still studying the relationship between estrogen and activity levels. However, some studies suggest estrogen replacement therapy may help you feel more motivated and may even increase your capacity to work out.
Why Exercise is Important During and After Menopause

Many women exercise less after menopause, but can estrogen replacement therapy help with exercising?
Before we learn more about how estrogen affects exercise, let’s talk about why exercise is so important as we get older and approach menopause. There are many reasons to be physically active throughout your life, including weight management, increasing muscle tone, getting stronger, and improving your overall health. Regular exercise is even more important as you reach menopause to help counteract certain health risks that increase around this time.
As hormone levels begin to decline, bone density and lean muscle mass begin to decline as well, while body fat can increase. Around this time in a woman’s life, there’s also a higher risk for many chronic diseases as well as cardiovascular disease. Engaging in an active lifestyle can help reduce these risks for many people. Regular physical activity helps promote bone health and muscle mass and can also help with body fat management. Exercise in later life can help improve and preserve flexibility and mobility and can also improve heart health. Regular exercise has also been linked to fewer instances of chronic diseases common as we get older.
In addition to physical health, exercise can also be helpful for other areas of well-being, such as mental health. Being physically active can also boost energy and mood and can even help combat some of the symptoms of menopause, such as insomnia. Overall, exercise can be an important part of maintaining quality of life as we get older.
Despite knowing that exercise is helpful for many areas of health, many women have a difficult time exercising on a regular basis, particularly after menopause. There may be many reasons for this, but some researchers believe hormonal imbalances may be a factor. Many studies are researching hormones, exercise, and whether estrogen replacement therapy after menopause can help improve activity levels for some women.
Estrogen Replacement Therapy Improves Menopause Symptoms that Make it Hard to Work Out
Menopause can cause many symptoms that can make everyday life difficult or even downright impossible. Hot flashes, insomnia, fatigue, and depression are all common symptoms of menopause that affect your quality of life. These also frequently make it difficult to exercise, which may explain why many women are more sedentary after menopause. It’s easy to understand why you might have a hard time going to the gym when you’re experiencing such troublesome symptoms. Working up a sweat can be anxiety-inducing if you’re already suffering from frequent and severe hot flashes. Insomnia and fatigue can leave you feeling worn out, making a workout sound plain exhausting. Menopause depression can zap your motivation for getting your heart pumping with a quick exercise routine. This is one theory behind why lower activity levels tend to coincide with declining estrogen levels during menopause.
The good news is hormone replacement therapy relieves many women’s menopause symptoms. Hormone therapy helps replace some of the hormones lost during menopause, which may improve your symptoms. As menopause symptoms improve, many people find it easier to take part in regular exercise for your health and well-being. This may be one explanation behind why menopausal women who use estrogen replacement therapy tend to be more active than those who don’t according to research.
Hormone Replacement Therapy with Estrogen May Act on the Brain to Increase Exercise Motivation
However, there are other theories behind how hormones affect exercise after menopause. Some believe estrogen may have a more direct effect on exercise. A new study suggests estrogen may act on the brain to improve motivation for exercise. The study looked at estrogen levels and physical activity levels in female mice to determine if hormones play a role in exercise.
The urge to exercise begins in the brain. You feel motivated to exercise, so you act on that motivation. There are also many estrogen receptors in the brain, which may affect your impulse to work out. The study looked at how estrogen affected brain processes through a specific gene. Melanocortin-4 receptor gene (Mc4r), is a gene that plays an important role in energy regulation, food intake, body weight, and the motivation for physical activity. Estrogen binds to the Mc4r receptor and can help activate it. With higher estrogen levels, Mc4r caused increased protein production for the mice in the study. Those mice with higher estrogen levels tended to be more physically active than the mice with lower estrogen.
Researchers are still studying the effects of estrogen on the brain. However, the scientists in the study believe this may offer some evidence that estrogen is important for exercise motivation. The researchers noted that while the study involved mice, humans have similar anatomies, physiologies, and genetics. Therefore, they believe estrogen in humans may have similar effects on exercise and physical activities. They noted that their research may suggest that estrogen replacement therapy may help improve motivation levels for exercise for menopausal women.
Estrogen Replacement Therapy Can Increase Exercise Capacity
Menopause can also affect how difficult exercise is, which may explain why many women are less active after menopause. Research shows that menopause may reduce exercise tolerance and oxygen consumption during exercise. This can make it feel harder to exercise, often leading to feeling more breathless, feeling muscle weakness, and other symptoms of low exercise tolerance, which can be discouraging and lead many women to exercise less than before menopause.
One study looked at exercise capacity for women before and after menopause. The researchers looked at many different factors to determine exercise capacity, which is the maximum amount of activity you can keep up. Some of the factors included the dilation of blood vessels, maximum workload, and peak oxygen consumption. Some of the group received estrogen replacement therapy for three months. The study found that estrogen significantly increased exercise capacity based on the factors they measured. The HRT group even achieved similar results to the pre-menopausal women in the study after just three months of hormone therapy. Therefore, this is just one other way estrogen may help with exercise after menopause.
Hormone Imbalance Treatment and Menopause Care at HerKare
Our team at HerKare is committed to providing quality healthcare for women at all stages of life. We help with everything from hormone imbalance treatment to well woman care for patients of all ages. We believe in empowering women to take an active role in their health. Our clinic is owned and managed by women for women. We understand the need for convenient care from healthcare professionals that listen to you and take time to understand. Let us help you feel like yourself and feel good again. Book an appointment at one of our clinic locations to get started with the HerKare process.

by SXHH Marketing | Nov 19, 2021 | Menopause
Any type of vaginal bleeding after menopause is a sign to visit our gynecologist. Vaginal bleeding is not normal after you have reached menopause, which is 12 months without a period. If you’re experiencing postmenopausal bleeding, this is typically a symptom of an underlying health conditions, some of which can be serious or life-threatening. Let’s talk about what to do if you noticed postmenopausal bleeding, what to expect at our clinic, and some common causes of vaginal bleeding after menopause.
Vaginal Bleeding After Menopause? Visit our Gynecologist

Vaginal bleeding after menopause isn’t normal. Your gynecologist can help address your symptoms.
Any time you experience vaginal bleeding after menopause, it’s important to discuss your symptoms with a women’s health care professional. While there is no reason to panic, you should take abnormal vaginal bleeding seriously, whether you’re experiencing light spotting or heavy flow.
An estimated 4% to 11% of women experience postmenopausal bleeding for one reason or another. Many women mistakenly believe that a little bleeding after menopause is no cause for concern and put off getting healthcare. However, we advise scheduling a gynecological services appointment as soon as possible to talk about your symptoms. While it may be something benign, postmenopausal bleeding can also be a sign of serious conditions like endometrial cancer. It’s better to be safe than sorry, so talk to one of our providers about abnormal bleeding.
What Will the Gynecologist Do for Postmenopausal Bleeding?
It’s understandable that you might be concerned about visiting our gynecologist to talk about postmenopausal bleeding. We realize that knowing what to expect during your appointment can help you feel more prepared and may help you feel better before and during your appointment. If you’re experiencing vaginal bleeding after menopause, our treatment providers may recommend a few things to help with diagnosis. In addition to talking about your symptoms, medical history, and relevant family history, the gynecologist may recommend different exams and procedures to help find the root cause.
Our Gynecologist will Likely Perform a Pelvic Exam
If you’re experiencing abnormal vaginal bleeding, our gynecologist will typically perform a pelvic exam. Pelvic exams can help our providers assess the health of your reproductive organs, like the vagina, uterus, cervix, and ovaries. During the exam, our provider may also screen for cervical cancer with a Pap test if you have abnormal vaginal bleeding.
Our Gynecologist May Recommend an Ultrasound
In some cases, our gynecologist may recommend a pelvic ultrasound to get a closer look at your pelvic and to help determine the source of your postmenopausal bleeding. This ultrasound may be abdominal or it may be transvaginal. Transvaginal ultrasounds use a thin imaging “wand” placed inside the vagina to get more detailed pictures of your pelvic organs.
Our Gynecologist May Recommend Diagnostic Surgery
While less common, sometimes our doctors may recommend a diagnostic surgery called a hysteroscopy. This procedure allows the doctor to look inside your uterus with a small camera to look for potential causes of postmenopausal bleeding. During the procedure, the doctor may also take a tissue sample to send to the lab for testing to help diagnose the source of your abnormal vaginal bleeding.
Talk to Our Gynecologist about Possible Causes of Postmenopausal Bleeding
There may be many causes of your postmenopausal bleeding. Some of these causes are more serious than others. Visiting our women’s health clinic can help identify underlying causes of your postmenopausal vaginal bleeding and help determine a course of treatment to help relieve your symptoms.
Uterine or Cervical Polyps
Polyps are small, noncancerous growths. If you’re suffering from vaginal bleeding after menopause, polyps in the uterus or cervix may be to blame. Polyps can easily become irritated and bleed, which can lead to spotting or even heavy vaginal bleeding. Uterine and cervical polyps are pretty common and are unlikely to become malignant, but when they cause symptoms like vaginal bleeding, generally gynecologists recommend removing them with a surgical procedure.
Vaginal Atrophy
Low estrogen levels during menopause can cause vaginal atrophy, which is where the skin becomes thin and dry. Vaginal atrophy can make the vagina more delicate and more prone to tears which can lead to vaginal bleeding. For instance, if you experience vaginal bleeding after sex, it may be due to friction. If this is the cause of your postmenopausal bleeding, our treatment providers may recommend vaginal moisturizers, vaginal estrogen, or lubricants to help.
Thickening Uterine Lining
In some cases, you may experience endometrial thickening after menopause that causes vaginal bleeding. This is called endometrial hyperplasia and while it is not cancer, it can increase your risk for endometrial or uterine cancer. Depending on your risk factors, our gynecologist may recommend taking progesterone to thin out your uterine lining. For women with higher risks for cancer, you may consider a hysterectomy as treatment.
Some Medications
Certain medications can also cause vaginal bleeding as a side effect. For instance, some women experience postmenopausal bleeding when taking blood thinners. Postmenopausal women taking hormone replacement therapy can experience vaginal bleeding as a side effect for the first six months of treatment. If you’re experiencing bleeding after menopause due to medications, we may explore changing your medications or recommend closely monitoring your symptoms to see if they change or get worse to determine if you may benefit from changing medications.
Infections
While rarer, endometrial infections can cause inflammation and vaginal bleeding after menopause. Doctors will generally prescribe antibiotics to help treat bacterial uterine infections. After treatment, your symptoms such as abnormal vaginal bleeding or discharge should improve.
Sexually Transmitted Infections
Another rare cause of postmenopausal bleeding are sexually transmitted infections. Infections like chlamydia or gonorrhea can cause inflammation that may lead to abnormal vaginal bleeding. In these cases, treating the STI generally stops the postmenopausal bleeding.
Endometrial Cancer
While it’s rare, postmenopausal bleeding can be a sign of endometrial cancer. Endometrial cancer is a type of cancer that begins in the lining of the uterus. About 10% of women who experience postmenopausal bleeding have endometrial cancer. However, an estimated 90% of women with endometrial cancer experience postmenopausal vaginal bleeding. Therefore, while endometrial cancer isn’t a common cause of postmenopausal bleeding, it can be an early warning sign of endometrial cancer. When caught early, the five-year survival rate is approximately 95%. In later stages, the survival rate is much lower. Because of the seriousness of endometrial cancer, most doctors recommend visiting a gynecologist to talk about postmenopausal bleeding and any other symptoms you’re experiencing.
Gynecological and Women’s Health Care from HerKare
Our health professionals at HerKare are here to empower you to take control of your health. We provide total women’s health care for every stage of life. Whether you need preventative care or are experiencing concerning symptoms, we offer quality care in our warm, welcoming clinics. As a clinic owned and operated by women for women, we are here to provide health care that suits your lifestyle. Make an appointment at one of our clinics today.

by SXHH Marketing | Nov 5, 2021 | Hormone Replacement Therapy, Menopause
Many women notice that their sex drive starts to decline over time, particularly after menopause. In some cases, this may be due to lower testosterone levels. Testosterone is an important hormone in your body that plays a key role in libido. Some studies suggest that testosterone replacement therapy may help women improve low sex drive due to testosterone deficiency.

Testosterone replacement therapy may help increase your sex drive if you’re suffering from testosterone deficiency.
As we age, sex hormones like estrogen, progesterone, and testosterone start to decline. Testosterone is mostly made in your ovaries, though your adrenal glands, fat cells, and skin cells may also produce some testosterone. While women produce a lot less testosterone compared to men (about 1/10 to 1/20 the amount), low testosterone levels for women can still impact your health and your sex life.
Testosterone in Women
While we commonly think of testosterone as a male hormone, women also need testosterone for many reasons. Testosterone is necessary for producing red blood cells, maintaining bone density, and also plays an important role in sex drive. When it comes to libido, the hormone testosterone can act on our brains to increase sexual thoughts and desires. It can also increase blood flow to the genitals to enhance sensitivity in the vagina and clitoris. This may also affect libido as well as sexual satisfaction.
However, testosterone levels begin to decline as we age, particularly as we reach the perimenopause state in the late 30s and 40s. During this time, the ovaries start to slow down hormone production for testosterone, estrogen, and progesterone. This can cause hormone levels to fluctuate and gradually decline leading up to menopause. With lower testosterone levels in your body, you might experience symptoms like low libido. Researchers have found a connection between low testosterone in women and lower sex drive. Studies have even found that women with low testosterone may have less sex on average than those with normal testosterone levels. Because of this connection, many women’s hormone care programs include testosterone to help improve sex drive and overall quality of life.
How Does Testosterone Replacement Therapy Affect Sex Drive?
Low libido due to testosterone deficiency can be distressing for many women. Some people experience stress and even relationship problems because of libido changes. Therefore, decreased sex drive can affect your quality of life in many ways. Many people mistakenly believe that low sex drive is a normal part of aging, but this isn’t necessarily true. Low sex drive can be caused by treatable conditions, like hormone changes during menopause. For instance, testosterone replacement therapy may help improve your symptoms.
Researchers are still studying the effects of testosterone replacement therapy for women. However, several studies have examined the link between testosterone and sex drive in women with interesting results. Studies have found that testosterone replacement therapy can increase several factors of sex drive and sexual satisfaction for postmenopausal women with low testosterone. Research suggests that testosterone can increase sexual desire, arousal, orgasmic response, pleasure, and even self-image based on interview responses. After beginning testosterone, many study participants also feel less distressed about their sexual function. Therefore, the evidence suggests testosterone therapy may help women who experience severely low sex drive after menopause.
The North American Menopause Society (NAMS) recognizes that testosterone replacement therapy for women may help some women improve sexual function. While testosterone for women is an off-label use, doctors may prescribe it to help with sex drive and sexual function. If you begin using testosterone therapy, NAMS recommends using the lowest dose for the shortest amount of time to help with symptoms. They also recommend discussing the risks and benefits thoroughly with a medical provider. After discussing the particulars, you and our doctors may determine to use testosterone therapy for better sex drive during and after menopause.
How Does Testosterone Replacement Therapy for Low Libido in Women Work?
If you’re experiencing low sex drive, there may be many different factors at play. Sexual desire, arousal, and satisfaction are all very complex. Therefore, pinpointing the cause of low sex drive can be difficult. There may even be several different causes of your low libido. It’s also necessary to note that libido can change for many reasons and a lower sex drive occasionally isn’t necessarily abnormal. For instance, if you have a lower libido during a stressful project at work, but your symptoms improve after you complete the project, then you may have nothing to worry about. However, if you have persistent low libido that worries you or interferes with your quality of life, you should talk to one of our providers about your symptoms.
If you’re suffering from low libido, one of the first steps most doctors recommend is ruling out other causes. For instance, some other reasons you might experience low sex drive that aren’t related to testosterone include:
- Low estrogen
- Low progesterone
- Depression
- Anxiety
- Fatigue
- Vaginal dryness
- Painful sex
- Relationship problems
- Some medications
- Other health problems like diabetes or hypothyroid
It’s important to identify underlying causes of low libido symptoms to find treatment solutions personalized to you. Some other treatments for severely low sex drive might include lifestyle changes, treating other health conditions, mental health treatments, or even couple’s counseling for relationship problems. For libido changes and other symptoms after menopause, our doctors may recommend beginning estrogen replacement therapy. If other treatments don’t work, or if no other explanation is found for your low sex drive, then it may be due to low testosterone levels. In these cases, you may benefit from testosterone replacement therapy.
Beginning Testosterone Replacement Therapy for Low Sex Drive
While considering potential causes of low sex drive, our providers may recommend performing a blood test to determine how much testosterone is in your blood. Normal testosterone levels for women are between 15 and 75 nanograms per deciliter (ng/dl). If you have low testosterone levels in your blood and you’re experiencing low sex drive that interferes with your life or causes you distress, our providers may recommend beginning testosterone replacement therapy.
The goal of testosterone replacement therapy is to bring testosterone levels to normal ranges. Because hormones like estrogen and testosterone hold each other in balance, it’s common to pair testosterone with estrogen replacement therapy as well to help prevent testosterone dominance. Therefore, in most cases your treatment program will include both estrogen and testosterone bioidentical hormones.
While taking testosterone treatments for sex drive, our team monitors your health to help optimize your treatment. We may track your symptoms, take blood draws to evaluate your testosterone levels, and assess other health markers like blood pressure and cholesterol levels. Our team also monitors you for common side effects of testosterone replacement therapy, such as increased facial and body hair, increased LDL cholesterol, or mild acne. Our goal is to help you feel your best and find treatment solutions that work for you and your lifestyle.
Quality Women’s Hormone Care at HerKare
Our team at HerKare offers quality health care for every stage of your life. After menopause, we understand that many of the symptoms can interfere with daily life. We offer personalized hormone care to help alleviate your symptoms so you can feel your best. Our clinics are owned and managed by women for women, and we believe in empowering you to address your health. We listen to you and work with you to get to the bottom of your symptoms. If you’re suffering from low sex drive or other menopause symptoms, help is available at our clinics. Make an appointment today to start the path toward feeling better.

by SXHH Marketing | Oct 20, 2021 | Menopause, Wellness
An estimated 75% of women will experience at least one vaginal yeast infection during their lifetimes. Some women experience yeast infections more frequently during and after menopause, often due to hormone changes. In some cases, other conditions you might experience during menopause can also increase the risk for vaginal infections like yeast infections. If you’re experiencing yeast infection symptoms, schedule a gynecological services appointment with our team to discuss diagnosis and treatment. Let’s go over some information you should know about yeast infections to help protect your health.
What is a Vaginal Yeast Infection?

Vaginal yeast infections are an overgrowth of yeast. Gynecological services can help with diagnosis and treatment of yeast infections.
First and foremost, you might be wondering what a vaginal yeast infection is. Many of us have heard of them or even experienced them without really knowing what they are. To understand what a yeast infection is, it’s important to understand that the vagina is like its own ecosystem. A healthy vagina typically has an acidic pH with a balance of bacteria and yeast. Those bacteria and yeast actually help keep your vagina healthy! However, if the balance between them gets thrown off for one reason or another, then the yeast cells can start to multiply and take over. When this happens, you experience a yeast infection. If you think you have a yeast infection, gynecological services can help diagnose the problem and one of our providers can prescribe treatment for the yeast infection.
Symptoms of Yeast Infections
There are many signs that can point to a yeast infection. Some common symptoms include:
- Itching
- Swelling
- Redness
- Pain during sex
- Burning during urination
- Soreness
- Rash
- White, clumpy discharge (like cottage cheese)
- Watery discharge
However, it’s also important to keep in mind that other conditions can cause similar symptoms. This can make self-diagnosis tricky, which is why we recommend visiting one of our gynecological service providers if you’re experiencing yeast infection symptoms.
Causes of Yeast Infections
There are many potential causes of yeast infections. For instance, taking certain antibiotics can raise your risk for yeast infections because they can reduce the number of healthy bacteria in your vagina responsible for keeping yeast cells in check. Other common causes include stress, lack of sleep, and uncontrolled blood sugar if you have diabetes.
Hormone imbalances may also be a risk factor for yeast infections. Hormones can have a pretty big impact on your vagina’s delicate microbiome. Fluctuations in estrogen can lead to an overgrowth of yeast and eventually a yeast infection. Therefore, some women notice that they get yeast infections more often during perimenopause when hormone levels start to change. During this time period, vaginal atrophy is also pretty common, which can also increase your risk for vaginal infections. We’ll discuss these common menopause-related causes in more depth a little later.
In many cases it can be difficult to determine the exact cause of your yeast infection. Also, in some cases they may not be preventable. It’s important to talk to one of our gynecological treatment providers about your symptoms and what you can do to help avoid yeast infections. Some general tips involve following good hygiene practices, keeping your vulva clean and dry, and avoiding potentially irritating things like scented bath products. Our treatment providers can help determine other changes that may help your specific situation.
Why Get Gynecological Services for Yeast Infections?
Some women choose to self-diagnose and self-treat yeast infections with over the counter medications. However, our team generally recommends scheduling an appointment with a gynecological services provider if you think you have a yeast infection.
There are several reasons to visit one of our treatment providers for a yeast infection. Self-diagnosing a yeast infection can be quite difficult. Several studies have found that women frequently misdiagnose themselves with yeast infections. One study showed evidence that only 34% of the study participants who purchased over-the-counter yeast infection treatments had accurately diagnosed themselves with a yeast infection.
Many other conditions can have similar symptoms to yeast infections. For instance, bacterial vaginosis, urinary tract infections, or even allergies from soaps or skincare products. Seeing a doctor can help rule out other causes of your symptoms and help verify that you have a yeast infection. One way to diagnose a yeast infection is to perform a lab test of your discharge to look for an overgrowth of yeast cells.
In addition, most over-the-counter yeast infection treatments are geared toward the most common type of yeast that causes yeast infections. However, some women may have a yeast infection from another type of yeast. Therefore, OTC treatments may not work for you if your yeast infection is due to another strain of yeast. In these cases, one of our providers can help identify the specific type of yeast and prescribe treatments specifically for that type of yeast infection. This can help you get the right type of treatment rather than deal with ongoing symptoms from using the incorrect anti-fungal treatments.
Can Menopause Lead to Yeast Infections?
Vaginal yeast infections can occur at any age. However, some women notice they get more yeast infections during and after menopause. Some common conditions you may experience during menopause can increase your risk for yeast infections. In addition, some of the symptoms of menopause can make you more vulnerable to yeast infections.
Vaginal Atrophy
We mentioned vaginal atrophy earlier as a potential risk factor for vaginal infections. Vaginal atrophy occurs when the tissues of your vagina become thin and dry. It’s pretty common with low estrogen levels during and after menopause. Vaginal atrophy may increase the risk for yeast infections, as it can change your vagina’s pH, bacterial levels, and yeast levels. These changes from vaginal atrophy can make your vagina more vulnerable to yeast overgrowth and yeast infections.
Also, some women even mistake vaginal atrophy symptoms for yeast infections. Vaginal atrophy can cause itching, irritation, pain during sex, and several other similar symptoms to yeast infections. This can lead some women to believe they have a yeast infection when they don’t. Gynecological services such as a pelvic exam and lab testing of vaginal discharge can help determine if you have a yeast infection or if there may be other causes of your symptoms.
Other Common Conditions During Menopause that can Lead to Yeast Infections
Also, there are other conditions you might experience during menopause that can increase your risk for yeast infections. For instance, many women experience frequent urinary tract infections during menopause due to low estrogen levels and vaginal atrophy. The most common treatment for UTIs involves taking antibiotics, which, as we mentioned earlier, can increase the risk for yeast infections. If you’re struggling with frequent UTIs after menopause, you may also experience more frequent yeast infections due to the antibiotics.
In addition, poor sleep can lower your immune system and increase your risk for yeast infections. Many women experience poor sleep during menopause due to hot flashes and night sweats. Frequent sleep issues during menopause may lead to vaginal yeast infections as well. Therefore, there may be many factors at play if you’re experiencing yeast infections during menopause, such as menopause symptoms that can affect your health.
Gynecological Services Can Help Address Underlying Causes of Yeast Infections
Sometimes yeast infections just happen, but symptoms should go away with treatment. However, if you have four or more yeast infections per year, you might have chronic yeast infections. This is important to discuss with one of our women’s health care providers, as there may be underlying causes to chronic yeast infections.
Treating underlying conditions may help reduce the number of yeast infections you get. For instance, if you’re struggling with vaginal atrophy after menopause, we may recommend estrogen or vaginal creams to help moisturize and thicken vaginal tissues, which may help reduce the number of yeast infections you experience. In other cases, our providers may recommend taking yeast infection medications for a longer period of time to help with chronic yeast infections.
One of the first steps toward getting help for frequent yeast infections is scheduling an appointment for gynecological services from our team. Our providers can go over your medical history, symptoms, and perform examinations and tests to determine if there may be underlying causes to your yeast infections.
Quality Women’s Health Care and Gynecological Services at HerKare
Our professionals at HerKare are here to help you feel your best, whether you have chronic yeast infections or need preventative well woman care. We are a women’s health clinic owned and managed by women. We take time to listen and understand what you’re feeling to help provide quality care for a wide range of conditions, from gynecological concerns to menopause symptoms. Make an appointment today to discuss how we can help you address your health.